Diabetes Prevention and Management Strategies: Your Complete Guide

Living with diabetes—or wanting to prevent it—can feel overwhelming. However, with the right diabetes prevention and management strategies, you can take control of your health and live a full, active life. In fact, research shows that up to 90% of type 2 diabetes cases are preventable through lifestyle changes.
Whether you’re at risk for diabetes, have been recently diagnosed, or are managing the condition long-term, this comprehensive guide will provide you with actionable strategies to keep your blood sugar levels in check.
Understanding Diabetes: What You Need to Know
Before diving into prevention and management strategies, it’s important to understand what diabetes actually is.
What Is Diabetes?
Diabetes is a chronic condition that affects how your body processes blood sugar (glucose). When you have diabetes, your body either doesn’t produce enough insulin or can’t effectively use the insulin it produces. As a result, glucose builds up in your bloodstream instead of being absorbed by your cells.
Types of Diabetes
There are three main types of diabetes:
Type 1 Diabetes occurs when your immune system attacks insulin-producing cells in the pancreas. Consequently, your body produces little to no insulin. This type typically develops in childhood or adolescence, though it can appear at any age.
Type 2 Diabetes, on the other hand, is the most common form. It develops when your body becomes resistant to insulin or doesn’t produce enough. Unlike type 1, type 2 diabetes is largely preventable through lifestyle modifications.
Gestational Diabetes develops during pregnancy and usually resolves after childbirth. However, it increases your risk of developing type 2 diabetes later in life.
Risk Factors: Are You at Risk?
Understanding your risk factors is the first step toward effective diabetes prevention and management strategies.
Non-Modifiable Risk Factors
Certain risk factors are beyond your control:
- Age: Your risk increases after age 45
- Family history: Having a parent or sibling with diabetes raises your risk
- Ethnicity: African Americans, Hispanic/Latino Americans, Native Americans, and Asian Americans face higher risks
- Gestational diabetes history: Previous gestational diabetes increases future risk
Modifiable Risk Factors
Fortunately, many risk factors can be changed:
- Excess weight, particularly around the abdomen
- Physical inactivity and sedentary lifestyle
- Poor dietary habits high in processed foods and sugar
- High blood pressure (140/90 mmHg or higher)
- Abnormal cholesterol levels
- Prediabetes (blood sugar levels higher than normal but not yet diabetic)
Diabetes Prevention Strategies
The good news is that type 2 diabetes is largely preventable. Moreover, implementing these strategies can reduce your risk by up to 58%.
1. Achieve and Maintain a Healthy Weight
Without a doubt, weight management is one of the most effective diabetes prevention strategies.
Why it matters: Losing just 5-7% of your body weight can significantly reduce diabetes risk. For instance, if you weigh 200 pounds, losing 10-14 pounds makes a substantial difference.
Action steps:
- Set realistic, gradual weight loss goals (1-2 pounds per week)
- Track your food intake using apps or journals
- Focus on sustainable changes rather than crash diets
- Celebrate small victories along the way
2. Get Moving: The Power of Physical Activity
Regular exercise is crucial for diabetes prevention. In addition to helping with weight management, physical activity improves insulin sensitivity.
Recommended activity levels:
- 150 minutes of moderate-intensity exercise weekly (brisk walking, swimming, cycling)
- 75 minutes of vigorous activity (running, aerobic classes, sports)
- Strength training at least twice per week
Getting started:
First, choose activities you enjoy—you’re more likely to stick with them. Second, start small if you’re currently inactive. Even 10-minute walks make a difference. Third, gradually increase duration and intensity over time.
Practical tips:
- Take the stairs instead of the elevator
- Park farther from store entrances
- Walk during lunch breaks
- Join group fitness classes for accountability
- Use fitness trackers to monitor progress
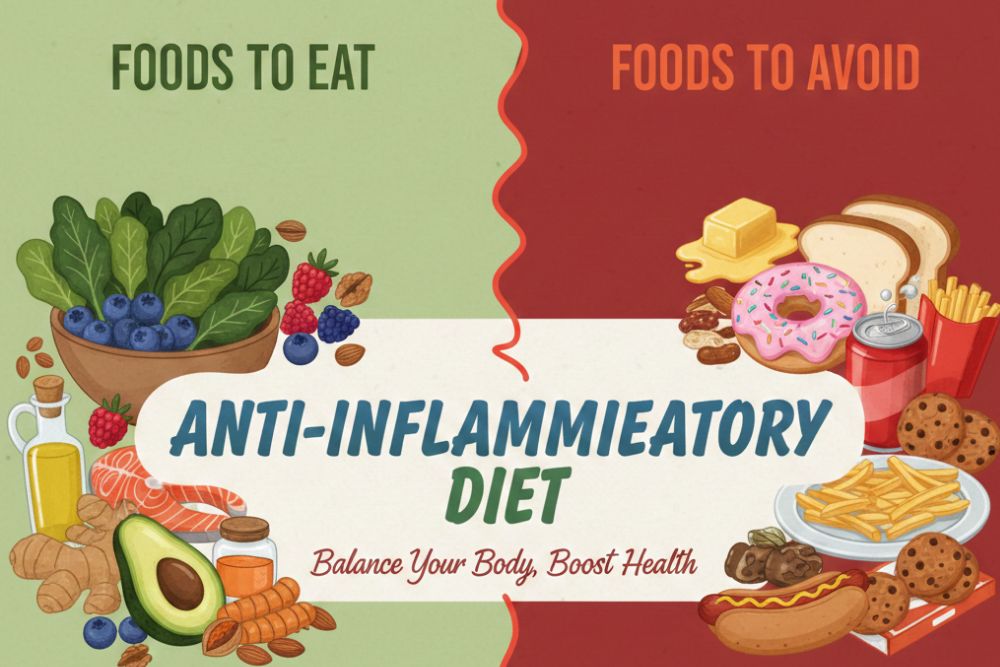
3. Eat a Diabetes-Preventing Diet
Nutrition plays a pivotal role in diabetes prevention and management strategies.
Foods to emphasize:
Fiber-rich foods help control blood sugar and promote fullness:
- Whole grains (brown rice, quinoa, oats)
- Legumes (beans, lentils, chickpeas)
- Vegetables (especially leafy greens)
- Fruits (berries, apples, pears)
- Nuts and seeds
Healthy fats improve insulin sensitivity:
- Avocados
- Olive oil
- Fatty fish (salmon, mackerel, sardines)
- Nuts (almonds, walnuts)
Lean proteins help stabilize blood sugar:
- Chicken and turkey
- Fish and seafood
- Tofu and tempeh
- Greek yogurt
- Eggs
Foods to limit:
- Sugary beverages (soda, sweetened coffee drinks, fruit juices)
- Refined carbohydrates (white bread, pastries, cookies)
- Processed meats (bacon, sausage, deli meats)
- Trans fats and excessive saturated fats
- High-sodium foods
Meal planning strategies:
Furthermore, how you structure your meals matters:
- Fill half your plate with non-starchy vegetables
- Allocate one-quarter to lean protein
- Reserve one-quarter for whole grains or starchy vegetables
- Practice portion control using smaller plates
- Eat regular meals to avoid blood sugar spikes
4. Stay Hydrated
Similarly, proper hydration supports diabetes prevention.
Why water matters: Drinking water instead of sugary beverages reduces calorie intake and helps kidneys flush out excess blood sugar.
Daily recommendations:
- Aim for 8-10 glasses (64-80 ounces) daily
- Drink more during exercise or hot weather
- Choose water, unsweetened tea, or sparkling water
- Limit alcohol consumption (maximum 1 drink for women, 2 for men daily)
5. Prioritise Quality Sleep
Interestingly, sleep quality directly impacts diabetes risk.
The connection: Poor sleep increases insulin resistance and appetite hormones. Studies show that sleeping less than 6 hours nightly raises diabetes risk by 28%.
Sleep hygiene tips:
- Maintain consistent sleep and wake times
- Create a dark, cool, quiet bedroom environment
- Avoid screens 1-2 hours before bed
- Limit caffeine after 2 PM
- Establish a relaxing bedtime routine
6. Manage Stress Effectively
Additionally, chronic stress elevates cortisol levels, which can increase blood sugar.
Stress-reduction techniques:
- Meditation and mindfulness: Even 10 minutes daily helps
- Deep breathing exercises: Practice 4-7-8 breathing
- Yoga: Combines movement with relaxation
- Time in nature: Regular outdoor exposure reduces stress
- Social connections: Maintain supportive relationships
- Hobbies: Engage in enjoyable activities
7. Regular Health Screenings
Lastly, early detection is key to prevention.
Recommended screenings:
- Blood glucose testing every 3 years starting at age 45 (or earlier if risk factors present)
- A1C test measures average blood sugar over 2-3 months
- Fasting blood sugar checks glucose after 8-hour fast
- Oral glucose tolerance test measures response to sugar intake
Normal ranges:
- Fasting blood sugar: Below 100 mg/dL
- A1C: Below 5.7%
- Oral glucose tolerance: Below 140 mg/dL
Diabetes Management Strategies
If you’ve been diagnosed with diabetes, these management strategies will help you maintain healthy blood sugar levels and prevent complications.
1. Monitor Blood Sugar Regularly
To begin with, consistent monitoring is essential for effective diabetes management.
Monitoring methods:
- Traditional glucose meters: Finger-prick testing
- Continuous glucose monitors (CGMs): Real-time tracking
- Flash glucose monitoring: Scan-based readings
Testing frequency:
- Type 1 diabetes: 4-10 times daily
- Type 2 diabetes (on insulin): As prescribed by your doctor
- Type 2 diabetes (medication): 1-2 times daily or as recommended
Tracking tips:
- Keep a detailed logbook or use apps
- Note patterns around meals, exercise, and stress
- Share data with your healthcare team
- Adjust habits based on trends
2. Follow Your Medication Plan
Furthermore, medication adherence is crucial for blood sugar control.
Common diabetes medications:
Metformin reduces glucose production in the liver and improves insulin sensitivity.
Sulfonylureas stimulate the pancreas to produce more insulin.
DPP-4 inhibitors help the body produce more insulin when blood sugar is high.
GLP-1 receptor agonists slow digestion and help pancreas produce insulin.
SGLT2 inhibitors help kidneys remove glucose through urine.
Insulin therapy may be necessary for type 1 or advanced type 2 diabetes.
Medication best practices:
- Take medications exactly as prescribed
- Don’t skip doses
- Understand potential side effects
- Inform your doctor about all supplements and over-the-counter medications
- Never adjust dosages without medical guidance
3. Master Carbohydrate Counting
Similarly, understanding carbohydrates helps manage blood sugar effectively.
Carbohydrate counting basics:
- Learn which foods contain carbohydrates
- Read nutrition labels carefully
- Measure portion sizes accurately
- Track carbohydrate intake at each meal
- Spread carbohydrates evenly throughout the day
Carbohydrate budgets:
- Women: 45-60 grams per meal
- Men: 60-75 grams per meal
- Adjust based on activity level and medication
The glycemic index (GI):
Moreover, choosing low-GI foods helps prevent blood sugar spikes:
- Low GI (55 or less): Most fruits, non-starchy vegetables, legumes
- Medium GI (56-69): Whole wheat, brown rice, sweet potatoes
- High GI (70+): White bread, white rice, sugary foods (limit these)
4. Build a Support Team
In addition, comprehensive diabetes care requires multiple healthcare professionals.
Your diabetes care team:
- Primary care physician: Oversees overall health
- Endocrinologist: Specializes in diabetes management
- Registered dietitian: Provides personalized nutrition guidance
- Diabetes educator: Teaches self-management skills
- Eye doctor: Monitors for diabetic retinopathy
- Podiatrist: Addresses foot health concerns
- Mental health professional: Supports emotional well-being
5. Prevent Complications
Consequently, proactive care prevents serious complications.
Essential preventive measures:
Foot care:
- Inspect feet daily for cuts, blisters, or redness
- Wash and moisturize feet daily
- Wear proper-fitting shoes
- Never walk barefoot
- Trim toenails carefully
- See a podiatrist regularly
Eye health:
- Schedule annual dilated eye exams
- Control blood pressure and cholesterol
- Quit smoking to protect vision
- Report vision changes immediately
Kidney protection:
- Monitor kidney function annually
- Keep blood pressure below 140/90 mmHg
- Limit protein if kidney disease develops
- Stay hydrated
Heart health:
- Take prescribed blood pressure and cholesterol medications
- Eat heart-healthy foods
- Exercise regularly
- Manage stress
- Avoid smoking
Nerve health:
- Report numbness, tingling, or pain
- Control blood sugar consistently
- Limit alcohol consumption
- Protect feet from injury
6. Handle Sick Days Carefully
Meanwhile, illness can affect blood sugar unpredictably.
Sick day guidelines:
- Check blood sugar more frequently (every 4 hours)
- Continue taking diabetes medications unless instructed otherwise
- Stay hydrated with water or sugar-free beverages
- Eat small, frequent meals if possible
- Test for ketones if blood sugar exceeds 240 mg/dL
- Contact your doctor if you can’t eat or drink, or if blood sugar remains high
7. Manage Blood Sugar Emergencies
Hypoglycemia (low blood sugar – below 70 mg/dL):
Symptoms: Shakiness, sweating, confusion, rapid heartbeat, dizziness
Treatment (15-15 rule):
- Consume 15 grams of fast-acting carbohydrates (4 glucose tablets, ½ cup juice, or 1 tablespoon honey)
- Wait 15 minutes
- Recheck blood sugar
- Repeat if still below 70 mg/dL
- Eat a meal or snack once levels normalize
Hyperglycemia (high blood sugar – above 180 mg/dL):
Symptoms: Frequent urination, increased thirst, blurred vision, fatigue, headaches
Treatment:
- Drink plenty of water
- Check for ketones
- Review recent food intake and medication
- Take prescribed rapid-acting insulin if applicable
- Contact your doctor if levels remain high or ketones are present
Creating Your Personalised Diabetes Action Plan
Now that you understand diabetes prevention and management strategies, it’s time to create your personalised plan.
Step 1: Set SMART Goals
Make your goals Specific, Measurable, Achievable, Relevant, and Time-bound.
Examples:
- “I will walk 30 minutes, 5 days per week for the next month”
- “I will reduce my A1C from 8.5% to 7.5% within 3 months”
- “I will lose 10 pounds in the next 8 weeks through diet and exercise”
Step 2: Track Your Progress
What to monitor:
- Blood sugar readings
- Weight and measurements
- Food intake
- Physical activity
- Medication adherence
- Mood and energy levels
Tracking tools:
- Smartphone apps (MySugr, Glucose Buddy, MyFitnessPal)
- Paper journals
- Spreadsheets
- Wearable fitness devices
Step 3: Adjust as Needed
Review and adjust:
- Assess progress weekly or monthly
- Identify what’s working and what isn’t
- Make necessary modifications
- Consult your healthcare team for guidance
- Be patient with yourself—change takes time
Lifestyle Modifications That Make a Difference
Quit Smoking
Above all, if you smoke, quitting is one of the most important diabetes prevention and management strategies.
Why it matters: Smoking increases insulin resistance and raises complication risks significantly.
Resources:
- Talk to your doctor about cessation medications
- Join support groups
- Try nicotine replacement therapy
- Use quit-smoking apps
- Consider counseling
Limit Alcohol Consumption
Similarly, alcohol affects blood sugar and can interfere with medications.
Safe drinking guidelines:
- Maximum 1 drink daily for women
- Maximum 2 drinks daily for men
- Always consume alcohol with food
- Monitor blood sugar closely
- Avoid sugary mixed drinks
Build Social Support
Additionally, social connections improve health outcomes.
Support strategies:
- Join diabetes support groups (online or in-person)
- Share your diagnosis with trusted friends and family
- Educate loved ones about diabetes
- Find an accountability partner
- Attend diabetes education workshops
Technology and Diabetes Management
Helpful Apps and Tools
Blood sugar tracking: MySugr, Glucose Buddy, One Drop
Nutrition and meal planning: MyFitnessPal, Carb Manager, PlateJoy
Fitness: Fitbit, Apple Health, Google Fit
Medication reminders: Medisafe, CareZone, Mango Health
Continuous Glucose Monitors (CGMs)
Benefits:
- Real-time blood sugar readings
- Trend analysis and predictions
- Fewer finger-prick tests
- Alerts for high or low blood sugar
- Data sharing with healthcare providers
Popular CGM systems: Dexcom, FreeStyle Libre, Guardian Connect
When to See Your Doctor
Contact your healthcare provider if you experience:
- Consistently high blood sugar levels (above 250 mg/dL)
- Frequent episodes of low blood sugar
- Symptoms of diabetic ketoacidosis (fruity breath, nausea, vomiting, confusion)
- Unexplained weight loss
- Persistent blurred vision
- Slow-healing wounds or infections
- Numbness or tingling in extremities
- Chest pain or shortness of breath
Conclusion: Taking Control of Your Health
Ultimately, implementing effective diabetes prevention and management strategies empowers you to take control of your health. Whether you’re working to prevent diabetes or managing an existing diagnosis, remember that small, consistent changes lead to significant results.
Start today by choosing one or two strategies from this guide. Perhaps you’ll begin with a 15-minute daily walk, or maybe you’ll focus on adding more vegetables to your meals. Whatever you choose, know that every positive step moves you closer to better health.
Remember, you’re not alone on this journey. Work closely with your healthcare team, lean on your support network, and be patient with yourself. With dedication and the right strategies, you can prevent diabetes or manage it successfully for years to come.
Frequently Asked Questions
Q: Can diabetes be reversed? A: Type 2 diabetes can sometimes go into remission through significant weight loss, dietary changes, and increased physical activity. However, this requires ongoing lifestyle maintenance. Type 1 diabetes cannot be reversed.
Q: How often should I check my blood sugar? A: This depends on your diabetes type, treatment plan, and blood sugar control. Your doctor will provide personalized recommendations, typically ranging from once daily to multiple times per day.
Q: Are artificial sweeteners safe for people with diabetes? A: Generally, yes. FDA-approved artificial sweeteners don’t raise blood sugar levels. However, moderation is key, and some people may experience digestive issues.
Q: Can I eat fruit if I have diabetes? A: Absolutely! Whole fruits contain fiber, vitamins, and minerals. Choose whole fruits over juices, watch portion sizes, and spread fruit intake throughout the day.
Q: How long does it take to see results from lifestyle changes? A: You may notice improved energy within days, while blood sugar improvements typically occur within 2-4 weeks. A1C changes usually take 2-3 months to reflect in testing.